:
• The discovery of Rh system is based on the work by Landstenier & wiener in 1940 & by Levine & Stetson in 1939.
• A woman who delivered a still- born foetus was transfused with her husband's blood. Although both husband & wife belonged to O blood group, the woman experinced a severe haemolytic reaction .
• Levine & Stetson proposed a theory that woman's red cells were lacking in an antigen & this antigen was called new antigen., which child had inherited from father.
• The antigen on foetal cells stimulated the production of antibodies in the mother's blood, so when she was transfused with husband's blood, these antibodies brought about haemolytic reaction.
• In 1940, Landsteiner & Wiener inoculated red cells of Rhesus monkey into rabbits & guinea pigs. The resulting antibodies agglutinated the red cells of monkeys & also of about 85% of the population.
These 85% were called Rh (Rhesus) positive because they possessed the same antigen that were present on red cells of Rhesus monkeys.
• The rest of the population were called Rhesus negative . Thus it was found that antibodies to same antigen can cause haemolytic reaction.
• The designation Rh is derived from the use of the blood of rhesus monkeys in the basic test for determining the presence of the Rh antigen in human blood.
• The Rh blood group system was discovered in 1940 by Karl Landsteiner and A.S. Weiner. Since that time a number of distinct Rh antigens have been identified, but the first and most common one, called RhD, causes the most severe immune reaction and is the primary determinant of the Rh trait.
Rh Antigen:
• The Rh blood group system has two sets of nomenclatures: one developed by Ronald Fisher and R. R. Race, the other by Wiener. Both systems reflected alternative theories of inheritance. The Fisher–Race system, which is more commonly in use today, uses the CDE nomenclature.
• This system was based on the theory that a separate gene controls the product of each corresponding antigen (e.g., a "D gene" produces D antigen, and so on). However, the d gene was hypothetical, not actual.
• The Wiener system used the Rh–Hr nomenclature. This system was based on the theory that there was one gene at a single locus on each of the 2 copies of chromosome 1, each contributing to production of multiple antigens. In this theory, a gene R1 is supposed to give rise to the “blood factors” Rh0, rh′, and rh″ (corresponding to modern nomenclature of the D, C, and E antigens) and the gene r to produce hr′ and hr″ (corresponding to modern nomenclature of the c and e antigens).
• The Rh blood group system is much more complex than ABO system. More than 40 antibodies have been describe
The proteins which carry the Rh antigens are transmembrane proteins, whose structure suggest that they are ion channels.
• The main antigens are D, C, E, c and e, which are encoded by two adjacent gene loci, the RHD gene which encodes the RhD protein with the D antigen (and variants)and the RHCE gene which encodes the RhCE protein with the C, E, c and e antigens (and variants).
• There is no d antigen. Lowercase "d" indicates the absence of the D antigen (the gene is usually deleted or otherwise nonfunctional).
• Thus, there are six related blood group factors C, D, E, c, d & e and corresponding antibodies (expect anti-d).
• Like ABO antigens , the Rh factors are also inherited traits. There are six Rhesus genes C, D ,E ,c, d & e.
• Thus there are only eight possible combinations in which chromosomes can carry these genes. they are CDe, cDE, CDE,cDe, Cde, cdE, CdE & cde.
A shorthand system has been devised for easy identification of these combination.
• The three pairs of genes are carried on the same chromosome & have three closely linked loci. Every individual has loci for six Rh genes.
• The factors C, D, E, c, d, & e (expect d) are antigenic. They are capable of stimulating the production of antibodies if introduced into the body of an individual whose red cells lack them.
• However Rh antigens vary in their degree of antigenicity. The D antigen is most immunogenic of them.
• The first transfusion of Rh (D) antigen into Rh (D) negative person will stimulate the production of anti D antibodies, thus subsequent transfusion with Rh (D) antigen will result in haemolytic transfusion reaction, similar to that of Levine & Stetson's patient in 1939.
• Thus it is necessary to test the blood of both donor & the recipent for Rh D antigen before blood trnasfusion. If blood sample shows presence of Rh (D) antigen it is considered as Rh positive or show absence considered as Rh negative.

The Du antigen:
• Some D antigens react weakly with anti-D sera. This weak reactivity with anti-D sera is due to Du antigen.
• Some workers belive that the presence of this antigen can be result of some genetic variation. One theory to explain Du antigen suggest that the D antigen is made up four fractions.
• An Rh-D positive individual possesses all four , while none is present in Rh-D ne
gative person.
• Some person may lack one or more of these fractions & therefore their red cells are agglutinated by only some of the anti-D antisera.
• Such incomplete D antigen is termed as Du . It does not usually react with complete anti-D, but it react with incomplete anti-D antisera with a varying degree of reactivity.
• While typing a blood sample for Rh antigen, the antierum will not produce agglutination with Du antigen, but will produce sensitized cells i.e the red cells will be coated with antibody.
The presence of sensitisied cells can be detected by the antiglobulin test.
• If Du person is given Rh-D positive blood, he or she is likely to produce anti-D antibodies therefore he or she is considered as Rh negative recipient.
• Similarly a Du person blood, when given to Rh negative person will stimulate anti-D antibodies.
• Therefore Du blood is given only to Rh positive persons.
A Coombs test, also known as antiglobulin test (AGT) is either of two blood tests used in immunohematology. They are the direct and indirect Coombs tests. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells.
• Since these antibodies sometimes destroy red blood cells, a person can be anemic and this test can help clarify the condition. The indirect Coombs detects antibodies that are floating freely in the blood.These antibodies could act against certain red blood cells and the test can be done to diagnose reactions to a blood transfusion.
• The direct Coombs test is used to test for autoimmune hemolytic anemia—that is, a condition where the immune system breaks down red blood cells, leading to anemia.
The direct Coombs test is used to detect antibodies or complement proteins attached to the surface of red blood cells.
• To perform direct test, a blood sample is taken and the red blood cells are washed (removing the patient's own plasma and unbound antibodies from the red blood cells) and then incubated with anti-human globulin ("Coombs reagent").
• If the red cells then agglutinate, the direct Coombs test is positive, a visual indication that antibodies or complement proteins are bound to the surface of red blood cells and may be causing destruction of those cells.
• The indirect Coombs test is used in prenatal testing of pregnant women and in testing prior to a blood transfusion. The test detects antibodies against foreign red blood cells.
• In this case, serum is extracted from a blood sample taken from the patient. The serum is incubated with foreign red blood cells of known antigenicity. Finally, anti-human globulin is added. If agglutination occurs, the indirect Coombs test is positive.
• Rh antibodies:
• Unlike ABO antibodies ,there are no naturally occuring Rh antibodies. All Rh antibodies are immune antibodies ,resulting from specific antigenic stimulation. eg: transfusion, pregnancy or by injection of antigen.
• Because there are no natural Rh antibodies, antibody typing is not possible in Rh system. Therefore, all Rh typing methods depend upon antigen typing using known serum.
• Some Rh antibodies cannot be detected in saline suspension of red cells. However if a protein rich medium such as serum or albumin is used, the antibodies can agglutinate the respective red cells. such antibodies are called imcomplete or albumin active antibodies.
• Th Rh antibodies which can react even in saline solution are called complete or saline active antibodies.
• There is still another class of antibodies which can be demonstrated only by means of antihuman globulin or Coomb's reagent. Such antibodies are known as incomplete univalent antibodies
The size of antibody molecule is largely responsible for the differences in their reactivities.
• The saline active antibody molecules are of IgM type & are largest.
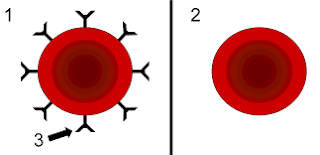
• The length of IgM molecule is sufficient to cause bridging of adjacent red cells in suspension. When in suspension red cells carry an electrical charge called zeta potential which causes repulsion among two adjacent red cells.
• The IgM antibody molecules extend beyond the range of zeta potential & agglutinate the red cells by binding onto their antigenic sites.
• The IgG molecules are smaller in size & cannot reach beyond the minimum distance between the cells, & are unable to agglutinate them.
• The zeta potential can be reduced by suspending the cells in high protein medium eg: patient own serum or 22% albumin solution.
• Similarly the antihuman globulin can detect incomplete univalent antibodies by bringing them together along with red cells to which they are attached.
• Rh typing Methods:
• As there are no naturally occuring Rh antibodies, Rh typing methods involve typing of red cells using known antisera against various Rh antigens.
• Commericial antisera are avaliable for C, D, E, c & e factors. since anti-d antibody is not known to be present. it is not possible to test for Rh-d factor.
• All blood sample which do not give positive reaction for Rh-D should be tested for Du antigen before reporting them as Rh-D negative.
• The method used for Rh-D typing depends upon the type of antibody used.
Method:1 Saline Method for Rh-D typing using complete Anti-D:
• A: Slide Test:
• Specimen : Whole blood or 50% red cell suspension prepared from clotted blood in patient own serum.
• Reagents: anti-D antiserum ( complete)
• Method:
1. Place a drop of antiserum on a labelled white tile.
2. Add two drops of specimen (whole blood or 50% red cell suspension).
3. Mix well & place the slide on a warm viewing box,to bring the temperature of mixture to about 370C.
4. Gently rotate the tile back & forth for a maximum of two minutes.
5. Examine microscopically for agglutination by transferring a small volume on slide with a clean pasteur pipette.
Test a positive & a negative control in the same way.
• Result:
• Agglutination: RhD positive.
• No agglutination: Rh-D negative
B: Tube Test:
• Specimen: Washed 5% red cell suspension of patient's blood.
• Reagent: Anti-D antiserum (complete)
Method:
1. In an appropriately labelled test tube add, one drop of anti-D antiserum.
2. Add one drop of 5% red cell suspension.
3. Mix well & incubate at 370C in a water bath for 30 minutes.
4. Roll the tube gently to redisperse the cells.
5. Check for agglutination microscopically. If no agglutination occurs, centrifuge at 200g for 1-2 minutes & check again.
6. Run known positive & negative controls simultaneously with test
Method 2: Albumin displacement technique for Rh typing using incomplete Anti-D:
• A 22% bovine albumin solution used in this method reduces the zeta potential (repllent electric charge) , thus bringing the red cells closer, so that IgG antibody molecules can agglutinate them.
• Specimen: 5% washed red cells suspension of patient blood.
Reagents:
• Incomplete anti-D antiserum.
• 22% bovine albumin.
Method:
1. In an appropriately labelled test tube, add one drop of incomplete anti-D & one drop of 5% red cell suspension.
2. Mix well & incubate at 370C in water bath for 60 minutes.
3. Without distrubing the cell button , run down one drop of 20% bovine albumin along the side of the tube onto cells. Do not mix.
4. Incubate further at 370C for 30 minutes.
5. Read microscopically for agglutination.
6. Run positive & negative controls simultaneously with test.
Method:3 Enzyme Techniques:
• Some antibodies aglutinate or lyse red cells which been treated with proteolytic enzymes such as papain, trypsin or bromeline.
• These enzymes remove some negatively charged molecules from red cells surface, allowing them to come closer for IgG molecules to agglutinate them.
• These proteolytic enzymes also increase agglutination by removing a part of hydration layer surrounding the red cells.